Save your child with your own hands
Here are some techniques to face unforeseen situations and help to save the ones you love.



Elisabete was at home, in the family office with her son, just 7 days old, on her lap. They were alone, and she had just finished breastfeeding Bruno. Suddenly, he started flailing his arms, shaking his entire body. His face turned red and he didn't make a sound. “I shook my son several times to make him cry. I thought: If he reacts, I know he's fine”, recalls Elisabete, who got in panic at that time. Fortunately, Bruno cried.
“First time” mother, Elisabete Strøm, 33 years old, had no idea how to act in situations like those. Even though she works in the health sector – she is a Physical Education teacher and former owner of a pharmacy in Feira de Santana, Bahia – taking care of a baby had never been part of her routine.
Elisabete told her husband, 39-year-old Norwegian Torbjørn Strøm, what had happened that morning, who calmed her down. However, when the boy turned 1 month old, another dangerous choking situation occurred. It was around 3:00am in the morning when Bruno woke up hungry.
She looked at her son's face when, once again, he stopped breastfeeding, turned red, and had his eyes widened. This time he coughed. In a few seconds, the young mother thought quickly and patted her son's chest. When it didn't help, she laid him face down on her lap and alternated patting his back with light pressure on his chest. Bruno swallowed and started breathing again.
“I could only cry and try to maneuver while praying to God for my son to catch his breath. Despite my despair, I managed to be rational.” Although Bruno recovered, Elisabete lost sleep. She decided that she couldn't bear a situation like that again without knowing exactly what to do. She spent the rest of that night on the Internet and got surprised with the number of reports of choking and deaths she founded out.
To help parents, here we present techniques and maneuvers that can help you save your child, explained by Dr. Aramis Lopes Neto, president of the Scientific Department of Safety of the Brazilian Society of Pediatrics, and by Dr. Paulo Carvalho, professor of the Department of Pediatrics and Childcare of the Faculty of Medicine, at the UFRGS.
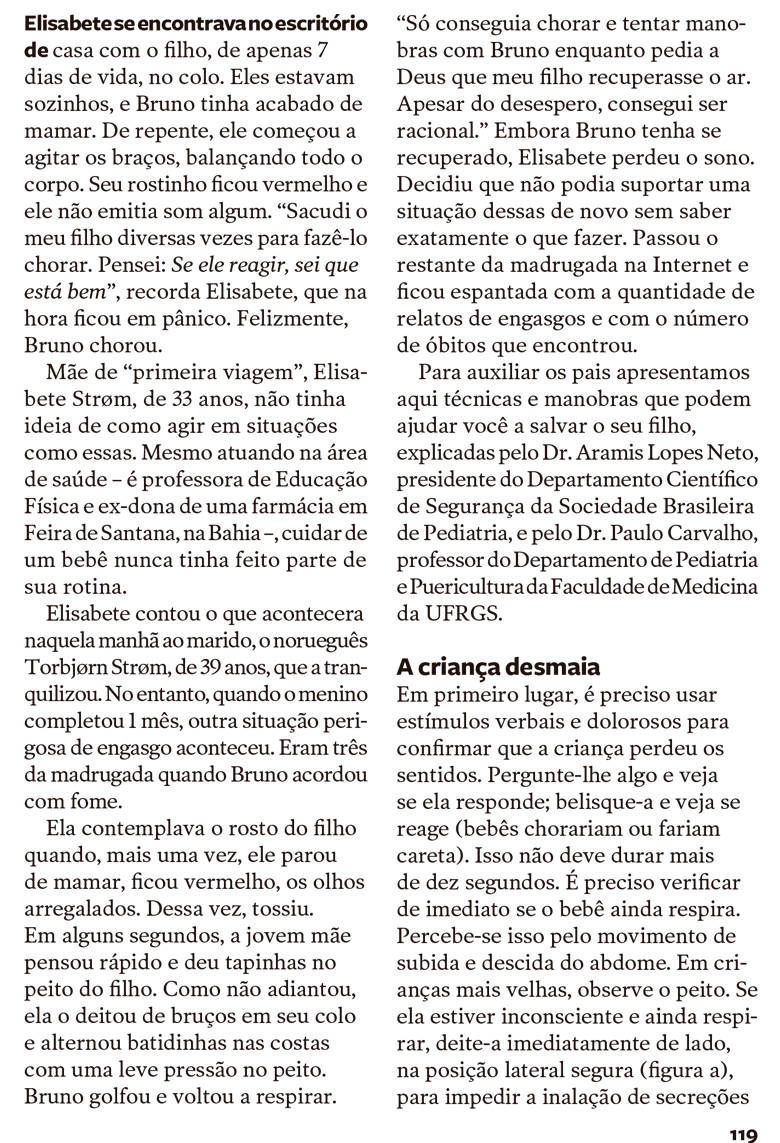
First of all, verbal and painful stimuli must be used to confirm that the child has lost consciousness. Ask them anything and see if they respond; pinch them and see if they react (babies would cry or grimace). This can't last any longer than 10 seconds. It is necessary to check immediately whether the baby is still breathing. This can be seen by the movement of the abdomen rising and falling. In older children, observe the chest. If they are unconscious and still breathing, immediately lay them on their side in the safe lateral position (figure a) to prevent inhalation of secretions if there is vomiting, and keep them under observation. Call the Fire Department immediately (193 - in Brazil).
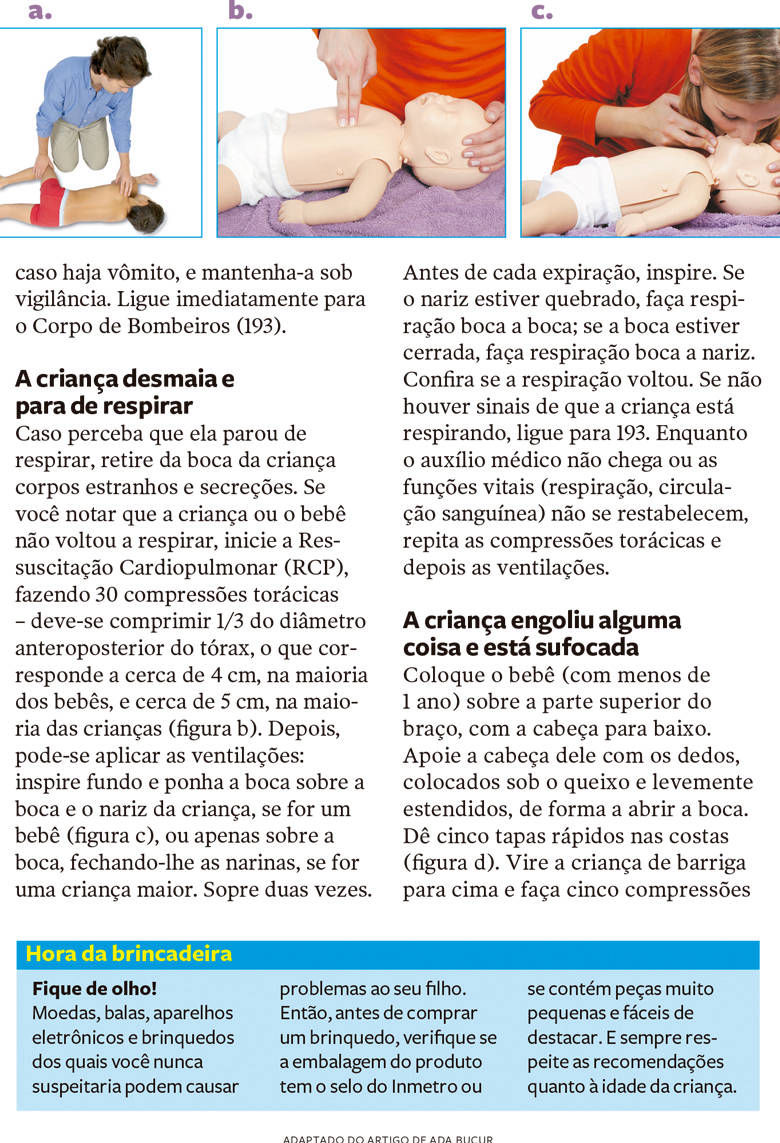
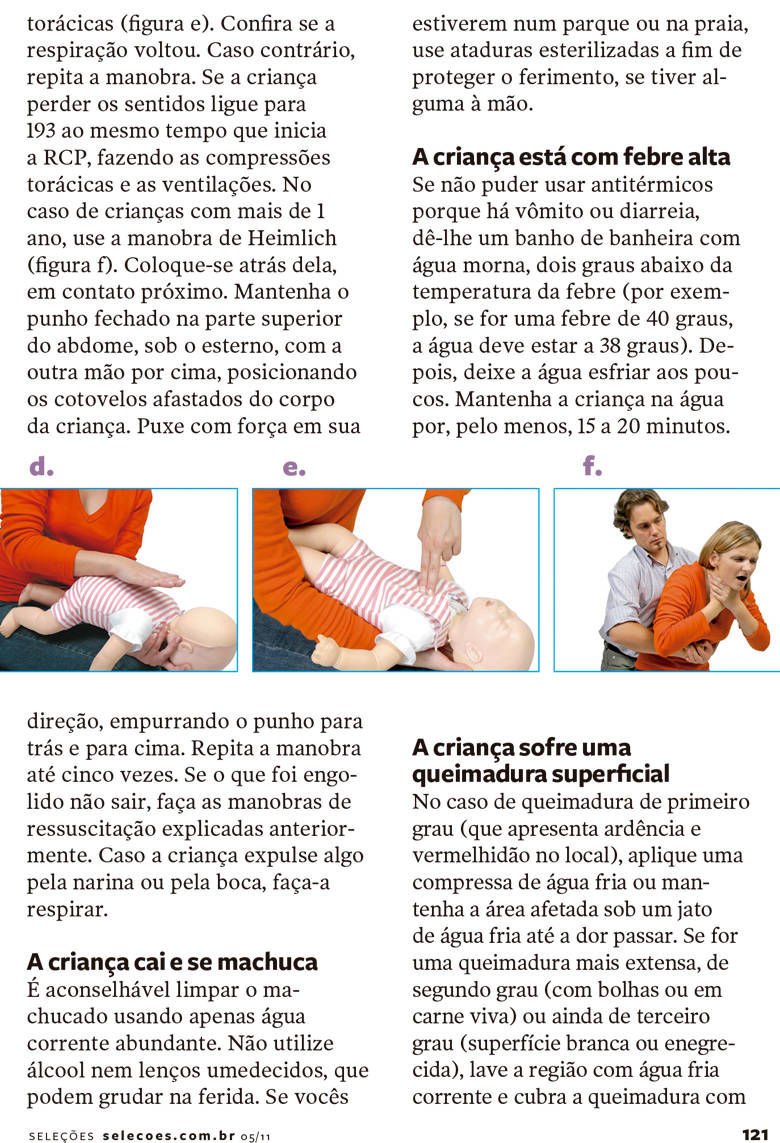
If you notice that the child has stopped breathing, remove foreign bodies and secretions from the child's mouth. If you notice that the child or baby has not started breathing again, start Cardiopulmonary Resuscitation (CPR), performing 30 chest compressions – you must compress 1/3 of the anteroposterior diameter of the chest, which corresponds to around 4 cm in most babies and around 5 cm in most children (figure b). Afterwards, ventilation can be performed: take a deep breath and place your mouth over the child's mouth and nose, if it is a baby (figure c), or just over the mouth, closing the nostrils, if it is an older child. Blow twice.
Before each exhale, inhale. If the nose is broken, perform mouth-to-mouth breathing; if the mouth is closed, try mouth-to-nose breathing. Check whether breathing has returned. If there are no signs that the child is breathing, call 193. Until medical help arrives or vital functions (breathing, blood circulation) are not restored, repeat chest compressions and then ventilation.
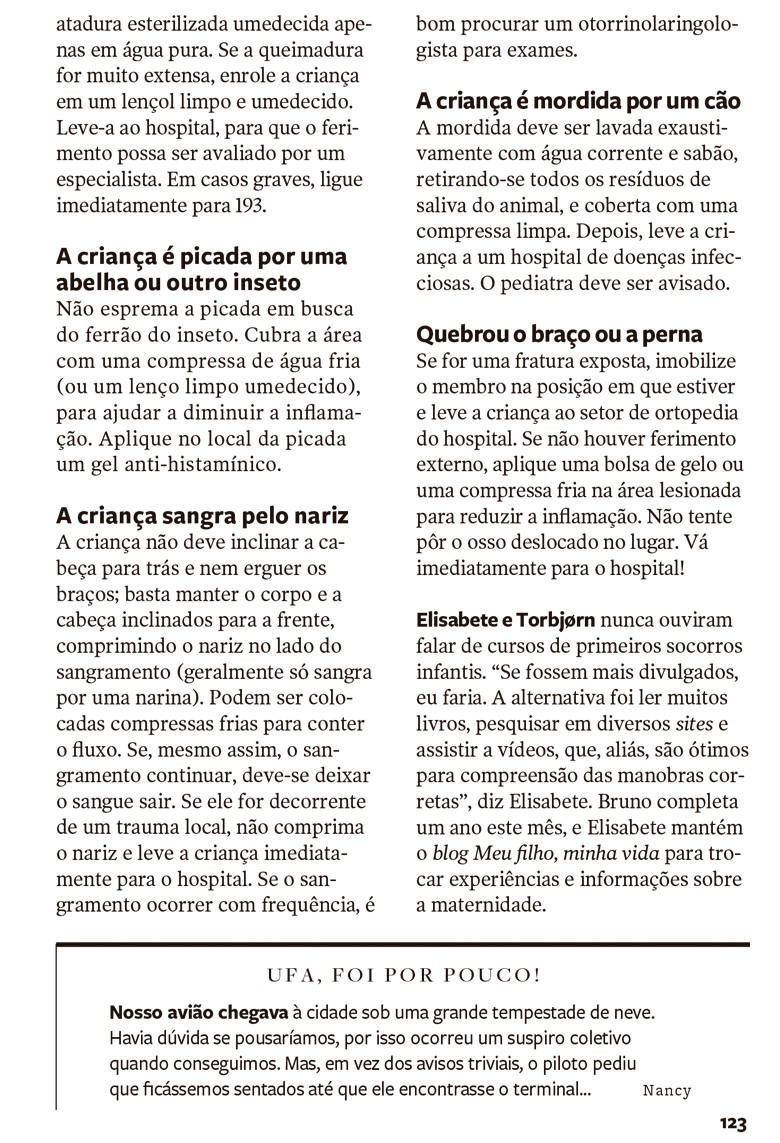
Place the baby (under 1 year old) on the upper arm, head down. Support their head with your fingers, placed under their chin and slightly extended, to open their mouth. Give five quick slaps on the back (figure d). Turn the child face up and perform five chest compressions (figure e). Check whether breathing has returned. If not, repeat the maneuver. If the child loses consciousness, call 193 at the same time as starting CPR, performing chest compressions and ventilation.
In the case of children over 1 year old, use the Heimlich maneuver (figure f). Place yourself behind them, in close contact. Keep a closed fist in the upper part of the abdomen, under the sternum, with the other hand on top, positioning the elbows away from the child's body. Pull hard toward you, pushing your wrist back and up. Repeat the maneuver up to five times. If what was swallowed does not come out, carry out the resuscitation maneuvers explained previously. If the child expels something through their nostrils or mouth, make them breathe.
Pay attention! Coins, candy, electronic devices, and toys that you would never suspect can cause problems for your child. So, before buying a toy, check if the product packaging has the Inmetro seal or if it contains very small parts that are easy to detach. And always respect the recommendations regarding the child’s age.
It is advisable to clean the wound using only plenty of running water. Do not use alcohol or wet wipes, which can stick to the wound. If you are at a park or beach, use sterile bandages to protect the wound, if you have any on hand.
If it is not possible to give antipyretics because there is vomiting or diarrhea, give them a bath with warm water, two degrees below the temperature of the fever (e.g. if it is a fever of 40 degrees, the water should be at 38 degrees). Then, let the water cool down little by little. Keep the child in the water for at least 15 to 20 minutes.
If its a first-degree burn (which presents burning and redness at the site), apply a cold water compress or keep the affected area under a stream of cold water until the pain subsides. If it is a more extensive burn, second-degree (with blisters or flesh) or even third-degree (white or blackened surface), wash the area with cold running water and cover the burn with a sterilised bandage moistened only in pure water. If the burn is very extensive, wrap the child in a clean and damp sheet. Take her to the hospital so the injury can be evaluated by a specialist. In serious cases, call 911 immediately.
BY SOLANGE KUPSKE RECH
Lorenzo was born in Dois Irmãos, in Rio Grande do Sul, on September 15, 2009. Soon after, Pediatrics consultations began and everything was going well. When my son turned six months old, in March 2010, we moved to my parents' house, in Giruá (RS). After that, I noticed a strange glow in Lorenzo's left eye that usually appeared at night, when the light from the lamp was reflected on it.
I decided to take my son to the health center. The doctor who examined him said it was just a reflex, as Lorenzo seemed healthy. But that “glow” continued and became more evident in a photograph. We came back to the same doctor, taking the photo with us and we were referred to an Ophthalmologist, but the appointment would be through the SUS and we would have to wait. Four months later, I mentioned Lorenzo's eye to a neighbour:
“It can be cancer! I've read it in a magazine!", she said.
What a fright! I thought he would have to wear glasses, that he would be squinting, but cancer? I have never imagined. My neighbour, a Seleções subscriber, showed us the article “The photo that saved a baby's life”, from the February 2010 edition.
I saw that the baby's eye was similar to my son's, I was sure that Lorenzo had retinoblastoma. We set an appointment with the ophthalmologist, Dr. Carlos Fernando Veroneze, and took the magazine with us. He said that only tests could give us any certainty, and requested an ultrasound of the eyeball. The result showed an expansive lesion on the left side, suggestive of retinoblastoma. Still, we wanted to get a second opinion. We went to Dr. Mateus Heicoff's. He examined Lorenzo and sent us to Hospital das Clínicas, in Porto Alegre. My son would be evaluated by Dr. Marcelo Maestri's team.
It all happened very quickly: on August 2, 2010 Lorenzo was admitted to Hospital das Clínicas and “enucleation” was performed (removal of the eyeball. In Lorenzo’s case, the left one). It was the worst day of my life, but I found strength in a sentence that I have read in the article: “What is an eye, compared to a life?” At that time, he, 10 months and 19 days old, was being reborn!
Today Lorenzo is doing well and uses a temporary prosthesis in his left eye. He is 1 year and 6 months old, and the treatment, which did not require chemotherapy, is being carried out by the team of Dr. Marcelo and Dr. Simone Almeida Silestre. To Revista Seleções, my neighbour “Naia”, Giruá and the doctors, a very special thanks!
Do not squeeze the bite to look for the insect's stinger. Cover the area with a cold compress (or a clean, damp tissue) to help reduce inflammation. Apply an antihistamine gel to the bite site. If the child is allergic to insect bites, give them antihistamines medicines to relieve symptoms.
The child should not tilt their head back or raise their arms; just keep their body and head tilted forward, pressing their nose on the bleeding side (it usually only bleeds from one nostril). Cold compresses can be applied to contain the flow. If the bleeding still continues, the blood must be allowed to drain. If it is the result of local trauma, do not pinch the nose and take the child to the hospital immediately. If bleeding occurs frequently, it is a good idea to see an Otorhinolaryngologist for tests.
The bite must be washed thoroughly with running water and soap, removing all residual saliva from the animal, and covered with a clean compress. Then take the child to an infectious disease hospital. The child's Pediatrician must be notified.
If it is an open fracture, immobilise the limb in the position it is in and take the child to the hospital. If there is no external injury, apply an ice pack or cold compress to the injured area to reduce inflammation. Do not try to put a dislocated bone in place. Go to the hospital immediately!
Elisabete and Torbjørn had never heard of children's first aid courses. “If they were more propagated, I would do it. The alternative was to read a lot of books, research on different websites and watch videos, which, by the way, are great for understanding the correct maneuvers”, says Elisabete. Bruno turns one this month, and Elisabete maintains the blog Meu Filho, minha vida (My Son, My Life, in english) to exchange experiences and information about motherhood.